
Invasive Coronary Artery Disease Diagnosis
Angiography has been the main invasive coronary diagnosis method for a long time. The use of X-ray equipment and contrast agents makes it available in all catheterization laboratories. Although it is fairly fast and straight forward, it has several limitations:
- It provides a 2D view of a 3D structure
- It does not provide any information on the blood flow
- It is operator dependent
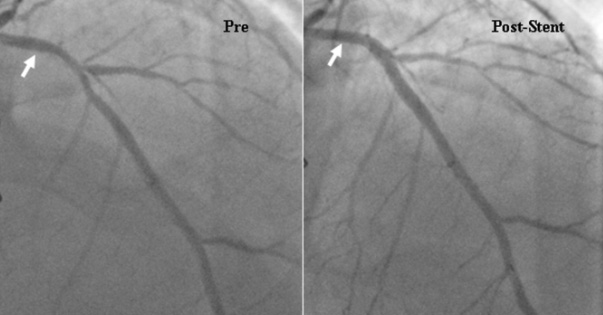
Interventional cardiology eventually started by assessing blood flow improvement and it was a logic turn when pressure guidewires came to market.
The landmark FAME study demonstrated that the use of Fractional Flow Reserve (FFR) improved clinical outcomes by reducing Major Adverse Cardiac Events by 28% vs. the use of angiography.1
FAME study: 1-year clinical outcomes1
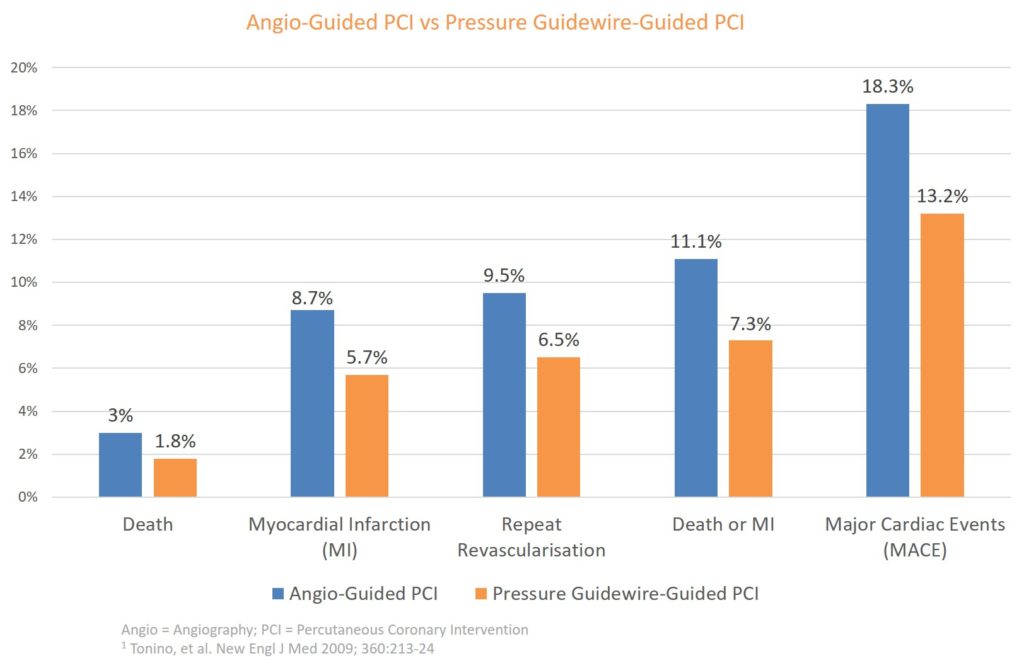
Pressure guidewires have been proven to be superior to angiography to diagnose coronary disease
- -28% Major Cardiac Adverse Events1
- >$2,000 Cost-Savings per Patient a Year
More studies have now been conducted showing the superiority of pressure guidewires over angiography in decision-making for Percutaneous Coronary Intervention (PCI). This has led cardiac societies to provide the highest recommendation to pressure guidewire usage for most indications.
Increasing Usage of Coronary Artery Physiology
Although pressure guidewires are highly recommended, their usage remains limited and mostly for 2 reasons: guidewire performance/lesion access and durability/accuracy.
There are currently 4 technologies available on the market:
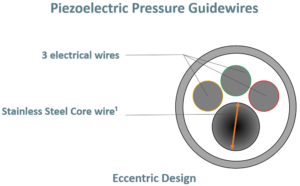
Piezoelectric pressure guidewires are the first technology that came to market over 10 years ago. The main limitations come from the sensor that requires electricity and the electrical cables that reduce the space available for the inner core, which translates into less torque and support, two key elements to navigate in the coronary arteries.
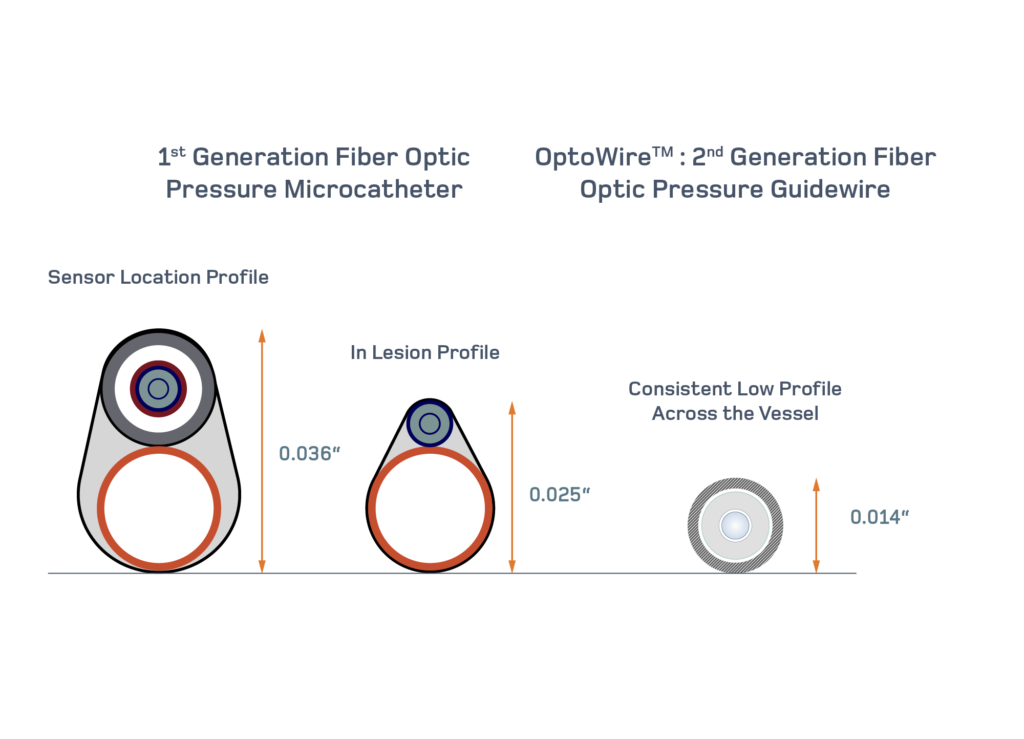
The microcatheter technology saw a lot of enthusiasm from cardiologists since it allowed them to use the workhorse guidewire of their choice and to slide the device over it to measure pressure. The size of the device is the key limiting factor as it can obstruct blood flow and has been reported to provide a wrong diagnosis to 1 in 5 patients5.
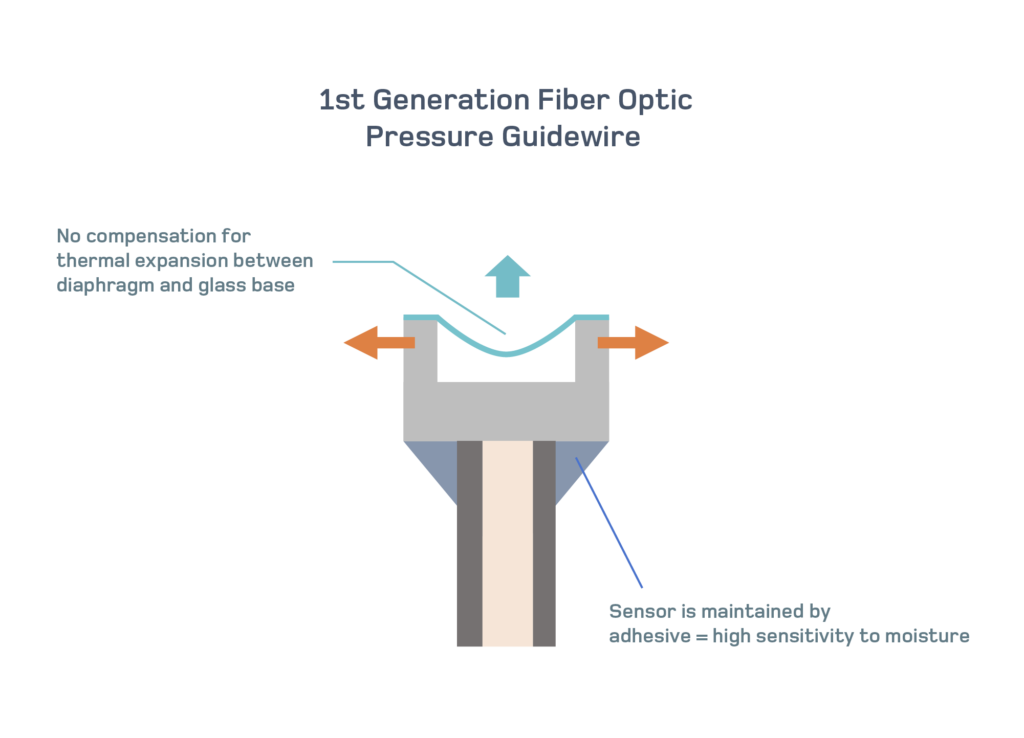
Came next, was the 1st generation fiber optic pressure guidewire, providing a much better performance to navigate the vessels. This advancement got limited by the lack of accuracy of the device. In one study they reported drift in 46% of the measurements3.
What is Drift?
An equalization is performed at the baseline to match the pressure guidewire measurement with the aortic pressure device, defined as 1.00. When physicians are done with the pressure guidewires, they should check in the same location if the guidewire and the aortic pressure device still have a match. Drift is defined by any final measurement equal or greater than 1.03 or equal or less than 0.97.
It has been reported that drift can change the diagnosis of 1 in 5 patients when using FFR and 1 in 4 patients when using a resting index7.
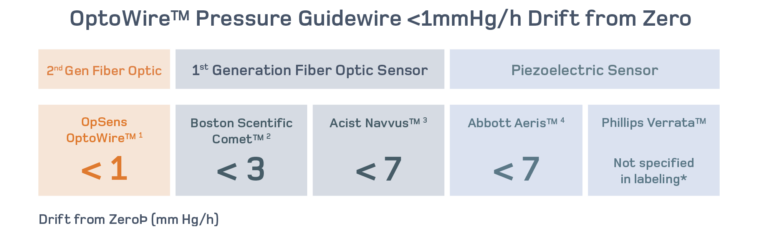
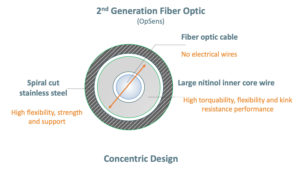
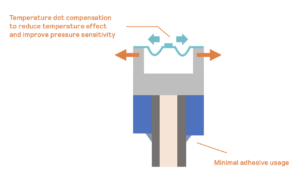
Finally, more modern pressure guidewires recently came to market with a 2nd generation fiber optic sensor. It is designed to provide the lowest drift in the industry with consistent and repeatable measurements.
Its large nitinol core and atraumatic tip with excellent shape retention provide unique guidewire control, torque and support.
OptoWireTM also has a disconnect/reconnect capability that helps take full control during complex cases with full confidence. It reconnects easily without re-equalization to make your measurements.
It also gives the ability to choose among different hyperemic and resting indices to assess coronary physiology.
Pressure Guidewires, 2nd Generation Fiber Optic Sensor

The OptoWire is a pressure guidewire, powered by FidelaTM, a 2nd generation fiber optic sensor. It has a design and performance that mimic very closely the design of a workhorse guidewire, making complex vessel navigation possible and predictable.
Additionally, the 2nd generation fiber optic sensor provides accuracy in the extreme conditions so physicians can use the same device to diagnose multiple segments ad arteries without worrying about losing accuracy.
Finally, this technology allows physicians to disconnect and reconnect easily to measure, perform PCI and confirm the improvement after the stent is implanted.
This last step could not be performed routinely before and has been reported to improve long-term clinical outcomes in several studies7,8.
Resting Indices
 We could not conclude this section without mentioning resting indices. FFR has been the gold standard in coronary physiology and requires hyperemia induced by drug such as adenosine to make the diagnosis. New indices that can be performed without the use of drugs have now come to market and have been proven to provide a good alternative to FFR9,10
Although they are much faster and easier to use, the scale to make a decision to treat is now narrower with an FFR cutoff value of 0.80 while the cutoff value for most resting indices is 0.89. In other words, while FFR provides 20 units to make a decision, resting indices provide only 11. The use of resting indices requires extreme accuracy, which makes the OptoWire perfectly suited for this kind of measurement. The OptoWire and OpSens diastolic pressure ratio (dPR) indice allows physicians to make several measurements, track the pressure variation across the artery (pullback) and assess pre-and post PCI with high confidence in the results’ accuracy.
The OptoWire brings physicians the possibility to diagnose and treat their patients with confidence.
We could not conclude this section without mentioning resting indices. FFR has been the gold standard in coronary physiology and requires hyperemia induced by drug such as adenosine to make the diagnosis. New indices that can be performed without the use of drugs have now come to market and have been proven to provide a good alternative to FFR9,10
Although they are much faster and easier to use, the scale to make a decision to treat is now narrower with an FFR cutoff value of 0.80 while the cutoff value for most resting indices is 0.89. In other words, while FFR provides 20 units to make a decision, resting indices provide only 11. The use of resting indices requires extreme accuracy, which makes the OptoWire perfectly suited for this kind of measurement. The OptoWire and OpSens diastolic pressure ratio (dPR) indice allows physicians to make several measurements, track the pressure variation across the artery (pullback) and assess pre-and post PCI with high confidence in the results’ accuracy.
The OptoWire brings physicians the possibility to diagnose and treat their patients with confidence. - Tonino, et al. New Engl J Med 2009; 360:213-24
- Fearon, et al. Circulation. 2018;137:480—487
- N.Curzen. Comet Study. PCR 2017. Study presentation.
- R. Tateishi. Comparison of accuracy of fractional flow reserve using optical sensor wire to conventional pressure wire. ESC 2018. Abstract presentation
- Pouillot et al, EuroIntervention 2018;13:e1850-e1856
- Agarwal, et al, Utilizing post-intervention fractional flow reserve to optimize acute results and the relationship to long-term outcomes. JACC Cardiovasc Interv.2016;9:1022—1031. doi: 10.101,6/j.jcin.2016.01.046
- Cook, et al. Circ Cardiovasc Interv. Feb 2017. DOI: 10.1161/ CIRCINTERVENTIONS.115.002988
- Hakeem et al., Post-PCI Pd/Pa and Outcomes, JACC Cardiovasc Interv. 2 0 1 9 : 2 0 0 2 — 1 4. doi: 10.1016/j.jcin.2019.07.0
- Davies et al, Define Flair, N Engl J Med 2017;376:1824-34. DOI: 10.1056/NEJMoa1700445
- Goetberg et al, Swedeheart, N Engl J Med 2017;376:1813-23. DOI: 10.1056/NEJMoa1616540

