CLINICAL CASE
By Giovanni Ciccarelli1 MD, Toru Tanigaki2 MD, Hitoshi Matsuo2 MD,PhD.
1 Clinica Mediterranea, Naples, Italy; 2 Department of Cardiovascular Medicine, Gifu Heart Center, Gifu – Japan
Easy to Use , Physical Bifurcation PCI, No drift
- Allows to perform complex procedures
- Evaluation of hyperemic and resting indices (dPR)
- Absence of drift
Case presentation
- 50-year-old man
- Risk factors: Dyslipidemia
- Presented with CCS Class II angina
- Coronary CT angiography: significant stenosis proximal LAD (Figure 1)
- Echocardiogram: normal ejection fraction
Angiography
Access via a right trans-radial approach with a diagnostic catheter.
Left coronary system (Figure 2):
- LM: aneurismal lesion and fistula with pulmonary artery
- LAD: significant lesion of the proximal and mid segment (Medina 1-1-0).
- LCx: no relevant stenosis.
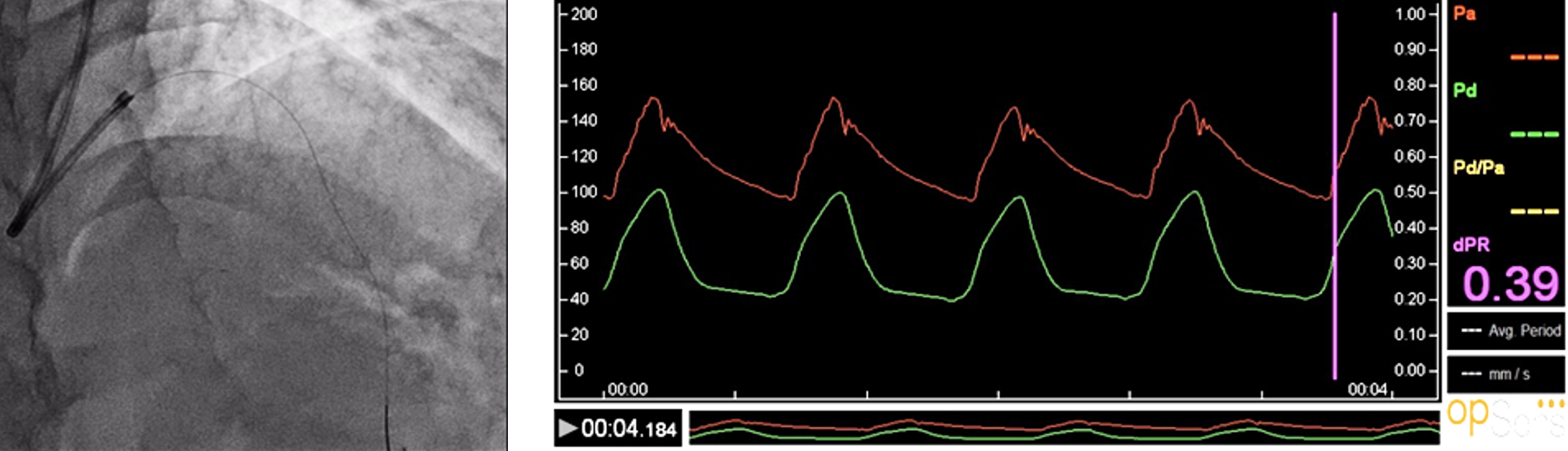
Pressure Measurements in Left Anterior Descending
- OpSens diastolic Pressure Ratio (dPR) was measured in both LAD (dPR 0.39) and diagonal branch (dPR 0.33), showing a significant stenosis, despite angiography showed a not significant stenosis of the diagonal branch.
Diagonal
Left anterior descending
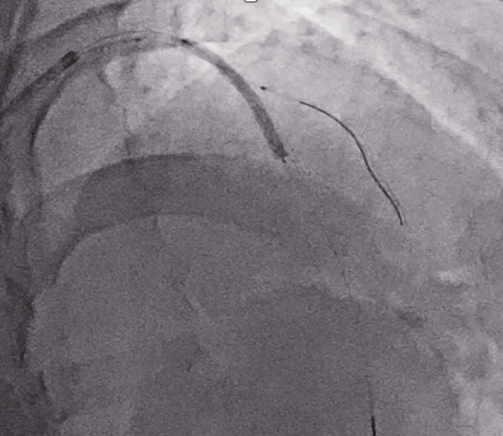
PCI of the prox/mid LAD was performed using a 7Fr Guiding over a workhorse wire, while a provisional OptoWire™ guidewire was positioned in the diagonal branch.
- 2.5 x 30 mm semi-compliant balloon over the OptoWire™ to protect the diagonal branch
- 3.0 x 32 mm everolimus bioabsorbable polymer stent was implanted in the prox/mid LAD.
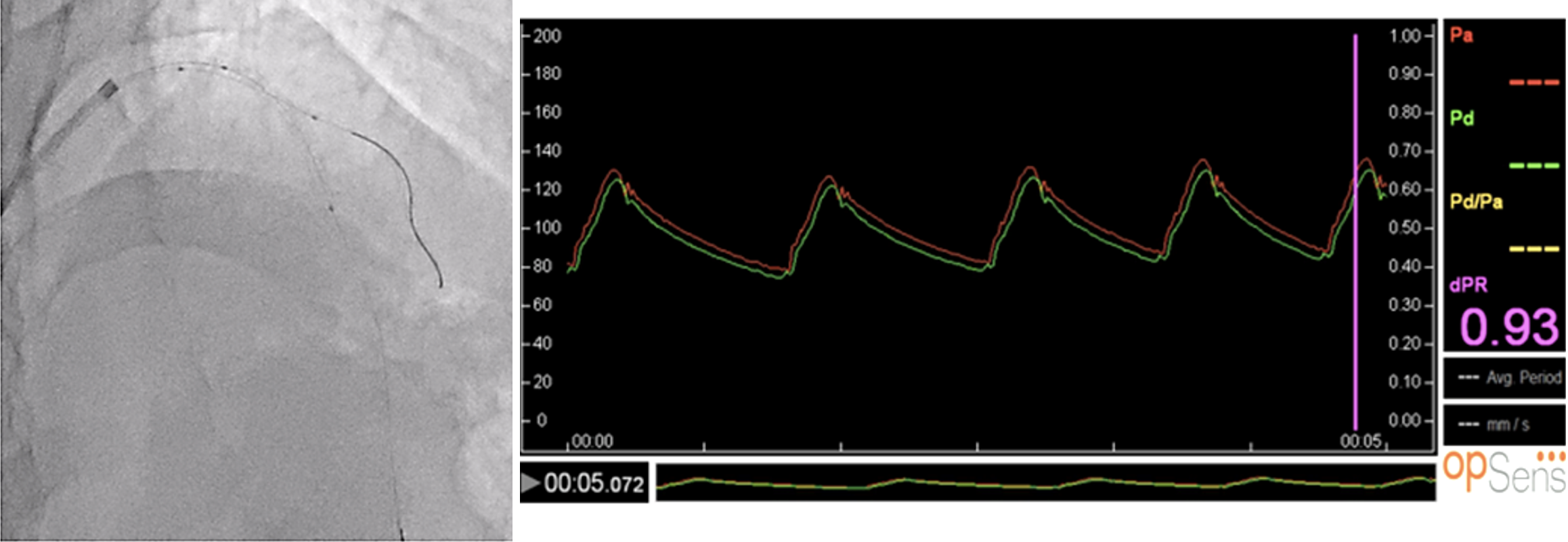
Post-PCI Pressure Measurements
After stent implantation, OpSens dPR was measured in the diagonal branch through the jailed OptoWire™, showing a negative value (dPR 0.93) (Figure 5). Then, LAD was wired with the OptoWire™ and a new physiological assessment was performed, confirming the optimal angiographic result (dPR 0.91) (Figure 6).
At the end of the procedure, pullback of the wire was done, and no drift was recorded.
Discussion
Physiological assessment of a coronary stenosis can better predict the clinical evolution as compared to angiography.1 Fractional Flow Reserve (FFR: hyperemic index) and Instantaneous wave Free Ratio (iFR: resting index) are recommended by the latest Guidelines to evaluate intermediate stenosis when evidence of ischemia assessed by non-invasive tests is not available.2-5
Recent studies have demonstrated that there is a substantial equivalence between all the resting indices.6
OptoWire™ guidewire is a 2nd generation fiber optic pressure guidewire enabled to evaluate both hyperemic (FFR) and resting (OpSens dPR) index to estimate physiological severity of coronary stenosis.
We were able to use OptoWire in the setting of a bifurcation PCI of the LAD-diagonal in 3 different steps:
- Evaluate the severity of the lesion
- Perform a provisional stenting of the bifurcation
- Compare the angiographic result to the physiological assessment post-PCI
At the end of the bifurcation PCI, no drift was recorded with OptoWire™ despite multiple disconnections and reconnections of the wir
Conclusions
The unique characteristics of the OptoWire™ guidewire allow interventional cardiologist to use it even in the setting of complex procedures like bifurcation PCI.
Using just one wire, we are able to decide if vessel revascularization was required, to perform a PCI and to evaluate the final result.
Opsens dPR is a new resting index feasible for clinical usage.
References:
- Ciccarelli G. et al, Angiography Versus Hemodynamics to Predict the Natural History of Coronary Stenoses: a FAME 2 Substudy, Circulation, 2018
- Tonino PA. et al, Fractional flow reserve versus angiography for guiding percutaneous coronary intervention, New England Journal of Medicine, 2009
- De Bruyne B, et al, Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease, New England Journal of Medicine, 2012
- Davies JE et al, Use of the Instantaneous Wave-free Ratio or Fractional Flow Reserve in PCI, New England Journal of Medicine, 2017
- Götberg M et al, Instantaneous Wave-free Ratio versus Fractional Flow Reserve to Guide PCI, New England Journal of Medicine, 2017
- Marcel van’t Veer et al, Comparison of Different Diastolic Resting Indexes to iFR: Are They All Equal?, Journal of American College of Cardiology. 2017